A new approach to risk adjustment
Optum® Prospective Solutions offers pre-visit and point-of-care support to help improve member outcomes. Our services support early detection and ongoing evaluation of chronic conditions for Medicare Advantage (MA), Affordable Care Act (ACA) and Medicaid members on behalf of health plans.
These services include:
- Prospective member assessments
- Digital integration strategy and implementation
- In-person and virtual support
- Member engagement campaigns
The Optum field team provides virtual and in-person support
The team is made up of 1,000 Health Care Advocates who work directly with 70,000 providers to manage gaps in care in all 50 states. They deliver wraparound services for providers that are customized to the level and type of support each practice requires.
We equip providers with actionable clinical insights, personalized member care gap information and administrative support. This helps create a workflow that prioritizes provider and member needs at the point of care and beyond. By reducing administrative burden, providers have more time to focus on clinical activities. In turn, this leads to better outcomes for members.
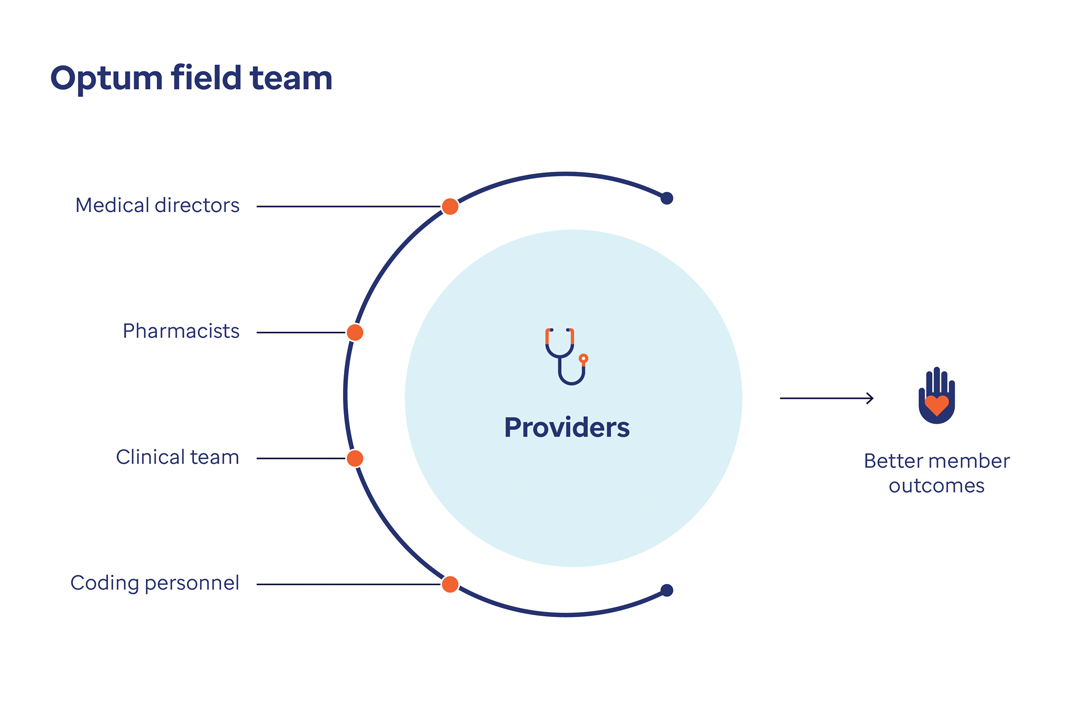
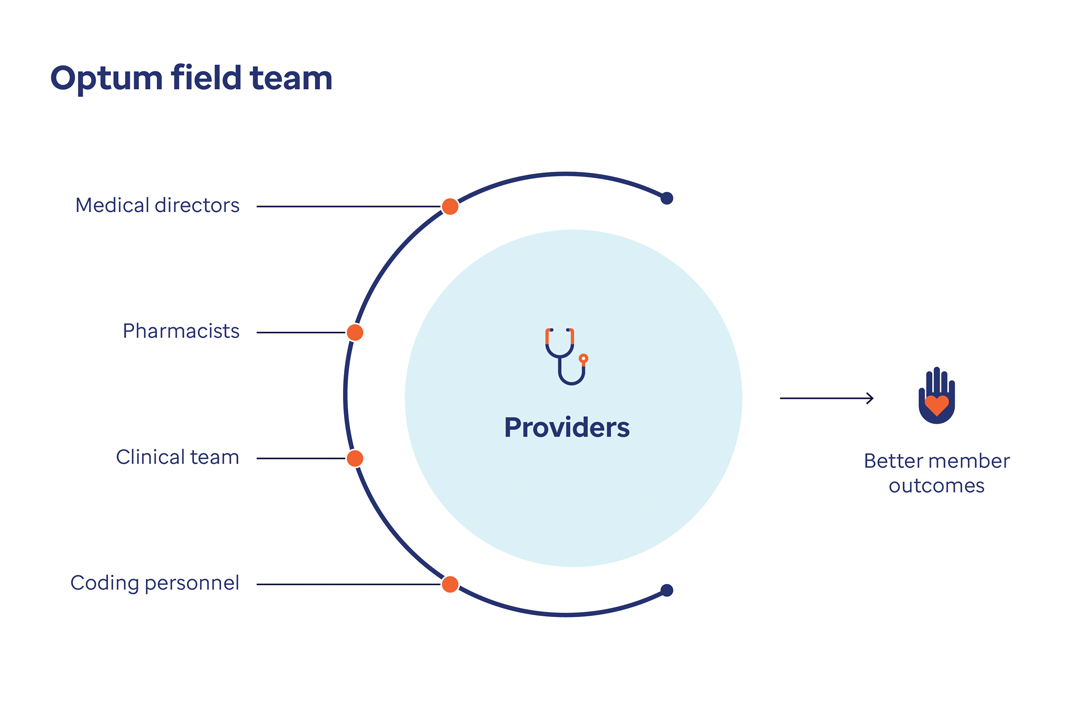
The Optum field team includes medical directors, pharmacists, the clinical team and personnel who help support providers. This support helps enable better member outcomes
Collaborative service model for payers and providers
Meet providers where they are with multiple modalities for prospective member assessment submission.
Native workflow integration
Providers can use their own internal tools and preferred resources to develop electronic workflows that fit their needs.
Practice Assist platform
This multi-payer, multi-program platform lets providers manage member care opportunities and program performance.
Integrated EHR applications
Providers can access risk suspects, quality gaps and supporting program documentation all within their native EHRs.
Partnership integrations
Optum partners with best-in-class, third-party technology services to offer providers even more options for digital assessment submission.
I have a caring relationship with my providers, we have the same goals … I’ve made an impact on the people I work with and they trust me.
Health Care Advocate, Optum
Learn about Prospective Solutions for providers
In-Office Assessment Program
We partner with physicians to support positive patient outcomes.
Risk Identification and Capture
Our holistic approach is designed to make it easy for clinicians to accurately document chronic conditions at the point of care.
Related healthcare insights
Article
Gain insights into how supporting providers can help increase engagement and reduce administration burden for better patient care.
Article
Step into the shoes of Richard Solomon, a Health Care Advocate, who goes above and beyond to support providers in risk adjustment programs.
Guide
Download our infographic to learn how Optum can take the burden off payers to impact provider performance.
Article
Discover the key elements to creating a positive, mutually beneficial relationship.
Case study
Empower provider success and improve member care through digital integration.
White paper
Learn how combining these steps can help power a holistic workflow between payers and care delivery.
Product information and resources
-
Download
PDF
Sell sheet
In-Office Assessment Program Overview
Learn about our provider-first model of collaboration, actionable data and interactive technology.
-
Download
PDF
Infographic
Prospective Risk and Quality Overview
Optum offers pre-visit and point-of-care support to help improve member outcomes. Download the placemat.



![Engage Providers to Impact Member Outcomes [Infographic]](/content/dam/o4-dam/images/professionals/providers/field-team-infographic-cover-1200x628.jpg)